Why Is Getting Sleep Apnea Diagnosed & Treated Critical To Your Health & Wellbeing? Links Below
Facts and Figures Why Get Treated
Positive Airway Pressure PAP Treatment
Quick Guides And Tips To Find & Fit The Right Mask
Facts and Figures of why to get your Snoring and Sleep Apnea Treated
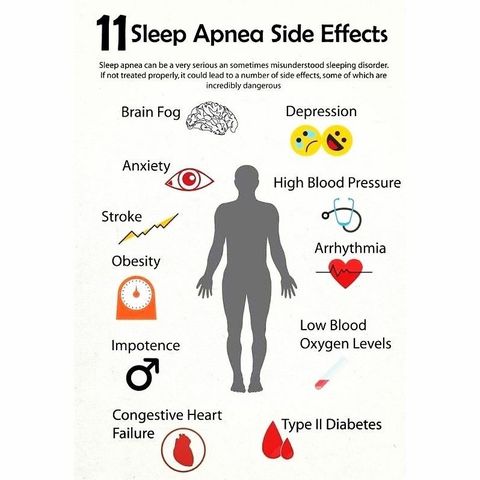
77% of those with Severe Obesity suffer with sleep apnea
73% of those with Congestive Heart Failure suffer with sleep apnea
72% of those with Type 2 Diabetes suffer with sleep apnea
50% of those with Atrial Fibrillation suffer with sleep apnea
35% of those with High Blood Pressure suffer with sleep apnea
30% of those with Coronary Artery Disease suffer with sleep apnea
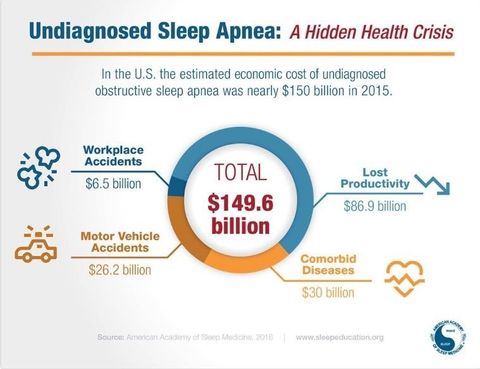
An individual with Sleep Apnea has a 68% increased chance of having a Stroke, a 58% increased chance of suffering from Depression and a 60% increased chance of having Metabolic Syndrome and Diabetes. 20% of the
population has Obstructive Sleep Apnea and Sleep Disturbed Breathing yet has no clue of its danger or existence because it, even today remains 90% undiagnosed. Those with no Sleep Apnea (an AHI less than five) have 96% chance of living another 18 years while those with Severe Sleep Apnea (an AHI over 30), have less than a 60% chance of living another 18 years.
AHI = Apnea Hypopneac Index and is the number of times you
quite breathing per hour. I have treated patients with AHI's from 5 to a range of 147 meaning this adult male ceased to breath 147 times/hour.
Health Risk Prevention
CPAP can prevent or reverse serious consequences of obstructive sleep apnea. The treatment can help protect you from these serious health risks. Studies report that after one year almost half of those prescribed CPAP fail to use it – after 5 years that number climbs to 83% intolerance. We have listed below the many health benifits to treating Sleep Disordered Breathing along with the value of CPAP in doing so! For those that fail CPAP, Oral Appliance Therapy (OAT) or a combination of CPAP and OAT very successfully treats this disease; so much so that for those mild to moderate cases OAT is recommended by both the Academy of Sleep Medicine and the Academy of Dental Sleep Medicine as the preferred treatment. Below you will find some of the risks of Obstructive sleep Apnea.
Heart disease
By treating your sleep apnea you can reduce your risk of heart disease. Sleep apnea is linked to a variety of heart problems because it causes you to stop breathing many times each night. These breathing pauses cause changes in your blood pressure and can reduce your blood oxygen levels. This puts an enormous strain on your heart. People with untreated sleep apnea have a higher rate of death from heart disease than those without sleep apnea or with treated sleep apnea. Using CPAP therapy over an extended period of time can protect you from heart problems and reduce your chances of dying from them. These heart problems include:
Congestive heart failure
Coronary artery disease
Irregular heartbeat
Stroke
If you have sleep apnea, consistent CPAP use can reduce your risk of stroke, one of the leading causes of death and long-term disability. A stroke is a sudden loss in brain function. It occurs when there is a blockage or rupture in one of the blood vessels leading to the brain. People with untreated sleep apnea are two to four times more likely to have a stroke.
Diabetes
Using CPAP to treat your sleep apnea can improve insulin sensitivity. Sleep apnea is related to glucose intolerance and insulin resistance, both factors in type 2 diabetes. Untreated sleep apnea increases your risk of getting type 2 diabetes.
Motor Vehicle Accidents
CPAP can help you become a safer driver by reducing your daytime sleepiness. Untreated sleep apnea makes you more likely to be involved in a deadly crash. Many people with sleep apnea have a hard time staying awake and concentrating while driving.
Benefits to Your Health and Well-Being
Using CPAP to treat your sleep apnea can improve your life and make each day better. It can help improve your overall health.
Daytime Alertness
Sleepiness and daytime fatigue are common symptoms of sleep apnea. CPAP can restore your normal sleep pattern and increase your total sleep time by eliminating breathing pauses in your sleep. This will help you wake up feeling more refreshed and boost your energy throughout the day.
Concentration
Untreated, severe sleep apnea can damage your brain tissue. As a result you may have trouble concentrating. You also may suffer from memory loss. Using CPAP may improve your ability to think, concentrate and make decisions. This also can improve your productivity and decrease your chance of making a costly mistake at work.
Emotional Stability
Untreated sleep apnea increases your risk of depression. CPAP can help improve your mood, reduce your risk of depression and improve your overall quality of life.
Snoring
By keeping your airway open as you sleep, CPAP reduces or eliminates the sound of your snoring. While you may not notice, you bed partner will benefit from a quieter sleep environment.
Medical Expenses
By improving your health, CPAP therapy can reduce your medical expenses. Sleep apnea can lead to more health problems and more doctors’ visits. Treatment for serious health risks linked to sleep apnea such as heart disease, stroke and diabetes can be costly. Medical expenses will decrease when you use CPAP to treat your sleep apnea.
History of CPAP
Many people may not realize it but author Charles Dickens played an instrumental role in defining what is now known today as Obstructive Sleep Apnea (OSA). In fact, in Dickens’ 1836 novel The Pickwick Papers there is a character called Joe, who is a “fat boy” who eats a lot and falls asleep in almost any situation. It is Dickens’ description of Joe’s sleep disorder that caught the eye of future doctors and researchers.
In 1918, Sir William Olser coined the term “Pickwickian” to describe patients who were not only obese but were sleepy all the time, sometimes napping involuntarily. And, in 1956, Dr. C.S. Burwell was treating patients who had congestive heart failure, extreme sleepiness or fatigue and improper airflow to the lungs. He began labeling these symptoms in patients as having Pickwickian Syndrome. Originally, it was thought that the sleepiness was a combination of excess weight and abnormally high levels of carbon dioxide in the blood. Then, in 1965 a group of French and German doctors lead by Dr. Henri Gastaut started doing research on patients with Pickwickian Syndrome. They recorded breathing and sleeping patterns and discovered distinctively unique patterns of apneas. Their research, along with future studies, eventually demonstrated that Pickwikian Syndrome is actually a breathing disorder caused by the position of the tongue and the tissues in the throat. As more information became available about the condition, Pickwickian Syndrome was later renamed Obstructive Sleep Apnea (OSA). They used the word apnea, which is a Greek word for breathless.
Doctors recognized that breathing was so difficult during sleep for patients with OSA that it could lead to death in some patients. At first, they weren’t sure how to treat the life-threatening aspects of OSA. But by 1969, doctors were treating severe cases of OSA with a tracheotomy to prevent people from dying while trying to sleep. This surgery allowed air to bypass the upper air passage altogether by creating an incision or opening in the trachea or windpipe and inserting a breathing tube. This practice continued for more than a decade. It wasn’t until 1981 that a less-invasive procedure became available for treating OSA.
An Australian researcher, Dr. Colin Sullivan, developed the first CPAP (Continuous Positive Airway Pressure) machine. This invention was a landmark development in the treatment of sleep apnea. The original machine contained a reversed vacuum cleaner motor that blew air into the affected person’s nasal passage using tubing to keep the airway open. Although the first CPAP machines were big, bulky and loud, by the late 1980s many improvements had been made to the machine and masks. It wasn’t long until the CPAP became the preferred treatment method for people with OSA. Since then, there have been steady technological improvements in the CPAP machine. For instance, the machines have become much smaller and quieter. And, the masks and straps are far more comfortable than the original machines. Additional features have been added to CPAP such as humidification to keep the airway from drying out, and self-adjusting air pressure levels that keeps pressures low early on to allow users to fall asleep and then adjust to the prescribed level during deep sleep.
BPAP is a model of PAP therapy that uses two different pressure settings, a higher pressure for inhalation and a lower pressure for exhalation. Today, the nasal CPAP is the “gold standard” for treating OSA. But to be effective, research shows the CPAP must be used every night for at least 4.5 hours on a routine basis. And yet one study showed that 50 percent of patients quit using the CPAP within the first year. Meanwhile another study found that patients only wear their masks about 40 percent of the time. While the reasons vary from person to person, most people still complain about inconvenience and discomfort. But finding a mask that fits properly can solve these problems. In the years that CPAP has become readily available numerous manufacturers and products has sprung up to accommodate different preferences. If you are having issues with your CPAP machine contact your doctor. It is better to resolve the issues and use the machine than it is to stop using it altogether. After all, your life could depend on it.
Positive Airway Pressure (PAP) Treatment
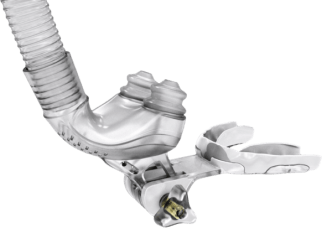
What is CPAP?
Continuous Positive Airway Pressure, or CPAP, is the treatment of choice for many people who suffer from obstructive sleep apnea (OSA). A CPAP device includes a small lightweight machine, tubing, nose mask, and headgear.
Who Needs CPAP?
CPAP is used to treat breathing disorders during sleep. People with central, mixed, and the more common obstructive sleep apnea may all benefit from CPAP therapy.
How Does CPAP Work?
During sleep, muscles in the airway relax, allowing collapse and any excessive tissue in the throat, such as tonsils, adenoids, tongue, or uvula, are allowed to then block the airway. These systems gently deliver machine-generated air into the airway through a nasal or full face mask. This air is positive pressure and acts as a splint to keep the airway open, thus eliminating obstructions. This provides immediate relief to OSA (Obstructive Sleep Apnea) sufferers by providing uninterrupted breathing and sleep. There are many different types of CPAP specifically designed to treat individual needs.
What is APAP or AutoPap
CPAP machines can only be set to one pressure setting that remains consistent throughout the night. Regardless of body position, weight loss or gain, or what stage of sleep you are in, the air pressure from a CPAP machine doesn't change. In other words, it does not have the capability of accounting for the sleep variability from night to night that we all experience. APAP on the other hand, has two settings, a low range setting and a high range setting, that the machine will fluctuate between throughout the night as it automatically adjusts itself to suit your needs at any given moment throughout your sleep. APAP machines use very sophisticated algorithms that sense subtle changes in your breathing needs and adjust themselves to the best pressure setting at any time of the night, while also adjusting for one’s needs night to night.
What is BiPAP?
BiPAP or bi-level therapy is similar to CPAP as it also provides positive airway pressure but at separate settings for inspiration and expiration. There is a higher pressure on inspiration, which prevents obstructions and facilitates airflow into the lungs. While during expiration there is a lower pressure that allows passive, easier exhaling while still maintaining an open airway. This method of treatment is useful for those patients that cannot tolerate the pressure of conventional CPAP therapy. In most cases a patient will need to try and fail at CPAP before a BiPAP will be prescribed.
What are some of the Side Effects or Complications of CPAP?
Nasal and throat dryness: Adding a humidifier to the system can prevent dryness.
Nasal Congestion: A heated humidifier can relieve most congestion.
Skin irritation from the mask: There are many different types of masks made from different materials to help prevent skin hypersensitivity. Changing to a different mask could solve the problem.
Pressure sores from the mask: This usually indicates that the mask is adjusted too tightly. The mask should only be snug enough to prevent leaks but loose enough to allow comfort. Different types and styles of masks should be explored to meet this goal.
Eye irritation: This may also result from an improper mask adjustment. Proper mask size, type and fitting may relieve this problem.
Claustrophobia: CPAP education and proper mask fitting can help to relieve anxiety and fear. Some CPAP units come with a “ramp” feature that allows the pressure to start gradually over the time it takes to fall asleep and then increases gradually to the therapeutic pressure needed to eliminate apneas. By the time the pressure has increased to the prescribed level, the person is asleep and unaware of the pressure change. This option must be discussed with a member of your medical team.
CPAP Intolerance: People who are unable to adjust and acclimate to CPAP therapy may benefit from bi-level therapy, which more closely mimics respiration and your breathing patterns. This option must likewise be discussed with a member of your medical team.
What are the benefits and how long is it needed?
The benefits of CPAP therapy are immediate but many times require a life-long commitment. CPAP is a treatment for apnea but not a cure! Apnea sufferers may try different treatment options, such as oral devices, medications, surgery or weight loss, but will probably not be cured by these options, either. These other treatments may decrease the severity of the breathing disorder, but CPAP has shown itself to be most effective if it can be tolerated by the patient. CPAP consistency, as with any other treatment, is the key to successful treatment of sleep apnea. It is imperative that people on CPAP use it every time they sleep. Because CPAP immediately eliminates apneas and obstructions, there is an improvement in sleep quality and oxygen levels in the blood. Once this happens, the symptoms associated with sleep apnea may subside. A person may feel rejuvenated, with an increased energy level, may feel less fatigued throughout the day, and may experience improved job/task performance. Treating sleep apnea may also decrease the risk for hypertension, heart attack and stroke. CPAP may also benefit sleep partners, since they won’t be bothered by snoring anymore.
How Can I Get a CPAP System?
An evaluation, sleep study and prescription are needed by a physician to get started on CPAP therapy. Once all of this has been completed, the physician will order the CPAP through a homecare company. The company provides the CPAP system and a nurse or respiratory therapist completes the initial set-up and education. Follow-up with the physician and the homecare company is needed to assess the progress and success of treatment.
Although CPAP is the most commonly prescribed therapy for those suffering with Obstructive Sleep Apnea, many people are unable to tolerate its use. Research says that 50% of those prescribed CPAP quite using it after the first year and that 83% quite by 5 years. Many times one's success can be improved by simply self advocating and being a "squeaky wheel" so to speak with the homecare company that provided the device. If unsuccessful there are other options such as Oral Appliances and a variety of surgical procedures.
Quick guides for all mask types:
Tips to Finding the Right Fit for Your CPAP Mask.
CPAP masks are all different and can be made by a variety of manufactures. For this reason, it is important to read the manufacturer’s material on the specific fit and features of your CPAP mask. Since we cannot go through each mask individually, we will discuss some universal rules to mask fittings and the problems that can arise during CPAP use. The most important thing to remember when using your CPAP mask is that it should not leak when in use. All masks have a small port to vent the air; in this area it is normal to feel air escaping the mask, and you should not worry. Leaks against your skin, however, need to be addressed so that your mask can work properly. If your mask does leak and you are not able to fix the problem, contact your home health provider and ask for assistance. The second most important thing to keep in mind is that tightening your mask is not always the solution to fixing a leak. It is possible to over-tighten a mask and make your problems worse. The masks are designed to be comfortable when worn, not to be painful. When fitting your mask, you want to make sure that the mask does fit snuggly to the face without being uncomfortable. The mask should not be so loose that it can slide around, but it should also not be so tight that it causes discomfort. If the mask has to be uncomfortably tight in order for any leaking to stop, contact your provider and discuss other mask options.
Nasal Pillows:
A nasal pillow is a small nasal mask that should sit right on the tip of your nose and seal around your nostrils. These masks are designed to be as small as possible while still delivering the pressurized air from the CPAP. It is important that the pillow portion of the mask correctly fits in your nose. Nasal prongs that are too big or too small can cause leaking and discomfort. The angle of the mask and its tightness are often the biggest obstacles to a comfortable fit. It is important to adjust all the straps of the mask individually so that an optimal fit can be achieved. These masks should not leak air onto your face or into your eyes. If they do,
adjust them again to see if the leaking can be stopped.
Nasal Masks:
A nasal mask is a small triangle-shaped mask that fits snuggly around the nose. These masks usually fit from the bridge of the nose down to the top of the upper lip. These masks may also have a small stabilizing bar that rests on the forehead. When fitting this mask, you want to make sure that the cushion (the softer gelatinous or plastic part) fits close to the actual size of your nose. You do not want your mask to be too large, leaving portions of your cheek s covered by the mask, neither do you want it to be too small, with the mask actually lying on the nose. It should fit into a nice triangle right along the outside of the nose. These masks tend to be easier to fit properly, and leaks are frequently taken care of with either a little adjustment to the mask angle or a small tightening of the headgear. If you have facial hair, however, this can interfere with mask fit. A mustache often will hinder the mask from fitting properly along the upper lip. Usually shaving or trimming the hair can help this problem.
Full-face Masks:
A full-face mask is a mask that fits from the middle of the chin area to the bridge of the nose, often with a stabilizing bar that sits on the forehead. As with all masks, sizing is very important. Your masks should not be too large or too long (falling off the end of your chin or lying too high on the bridge of your nose), nor should they be too small (hindering you from slightly opening your mouth). These masks often have an exhalation port on them where you will find a small leak so that the air can circulate in the mask. These masks should not leak onto the skin. If you do have leaks into the eyes or along your cheeks, or if you hear any noise coming from the mask, you should refit the mask again. Full-face masks should fit tightly on the face, but not too tightly. Small adjustments should be made to the straps to see if the leaking can be stopped. If the mask becomes painful or too tight, you should go to your provider and ask to be fitted again. Facial hair can cause a lot of leaking with these masks. Men with beards and mustaches may have difficulty getting these masks to fit with any leakage. If you do have facial hair, a good idea may be to shave some of it or to trim it to try to lessen the leak. As always, if you are having trouble with your mask or are getting discouraged about the fit, contact your home healthcare provider and seek assistance.
Quick Tips:
Sores or redness on the face: Soak the mask in warm water to make sure there is no build-up on the mask causing irritation. Also, check the size of the mask to make sure it is the correct size for your face. Make sure that you are not allergic to the materials in the mask.
Discomfort from tightness: Loosen the mask and check that the mask is fitting properly on your face. Check that facial hair or other skin problems are not causing the mask to leak.
Mask stiffness: Make sure to wash your mask often and take proper care of it. If the mask continues to be stiff or cracks, call your home health provider about ordering a new mask.
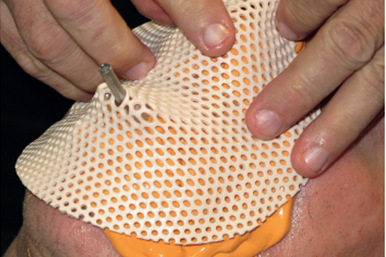
Custom Fabricated Masks
Many times, a primary patient complaint and reason for CPAP non-compliance is a poor fitting or leaking mask. A custom fabricated CPAP mask is a wonderful option for the patient who has “tried everything” available and still cannot get a comfortable fit and seal from an off the shelf mask. Custom CPAP masks are also ideal for special needs patients, as well as those patients with structural issues. The conveniences of the custom CPAP masks are:
- NO STRAPS! No straps are needed to keep the masks completely seated throughout the night, no matter the sleeping position.
- Virtually no air leakage, allowing the patient to receive their full therapeutic titrated pressure levels.
The masks can be used for patients receiving only CPAP therapy or in conjunction with oral appliance therapy. An oral appliance, when used in conjunction with the custom CPAP mask, allows CPAP pressures to be significantly lowered. This combination therapy is perfect for moderate to severe sleep apnea patients, who may struggle with high CPAP pressure settings.
Once it has been determined that a patient is a candidate for a Custom Fit Mask molds are made of the face and a custom mask is fabricated and anchored to an oral appliance. The pictures above will give you an idea of the process. Reach out to us should you think this suits your needs.
The content below is taken from some of Dr. Viviano's work ............
Dr. Viviano graduated from the University of Toronto in 1983. His clinic is limited to managing sleep-disordered breathing and sleep-related bruxism. He is a Credentialed Diplomate of the American Board of Dental Sleep Medicine and has lectured internationally, conducted original research, and authored original articles on the management of sleep-disordered breathing. His clinic is the first Canadian facility accredited by the American Academy of Dental Sleep Medicine and he is Clinical Director of the Sleep Disorders Dentistry Research and Learning Centre.
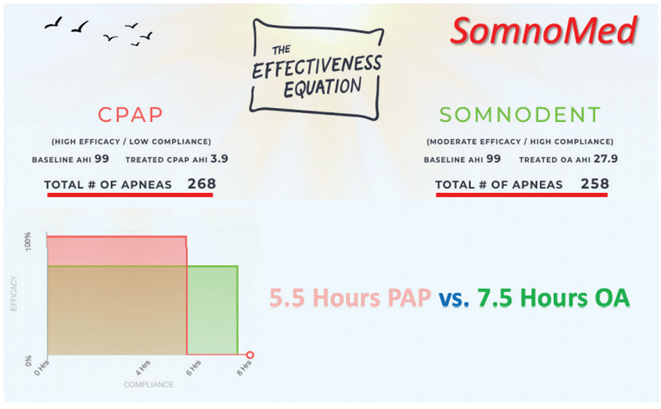
The two examples above demonstrate a similar concept as the paragraph and the graph to the right but presented in a little different context. We know:
- There are more breathing events in Rem Sleep than other sleep stages.
- The later the night goes the lengthier and the more Rem Sleep there is.
Conclusions:
- For a patient with an AHI of 99 who wears a CPAP 5.5 hours/night vs an Oral Appliance worn 7.5 hours/night, the Oral Appliance reduces the overall AHI better than the CPAP.
- For a patient with an AHI of 27.6 who wears a CPAP 5hours/night vs an Oral Appliance worn 7.5 hours/night, the Oral Appliance is equal to CPAP.
- This provides a strong argument for changing the prescribing patterns of physicians for their patients with OSA since we know 50% of those wearing PAP quit therapy after one year and 83% quit prior to five years.
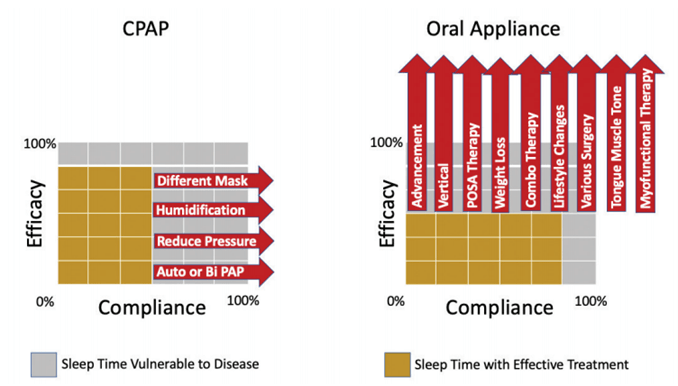
As can be seen from the right we can improve CPAP Compliance by trying different masks, adjusting the humidifier, reducing the pressure or if indicated switching from a CPAP to an AutoPap or BiPap. With Oral Appliances we can change Efficacy by adjusting the advancement, the amount of opening, adding positional therapy, combination therapy, encouraging lifestyle changes, improving tongue muscle tone or adding Myofunctional Therapy.
THE REALITY OF THE SITUATION
TROUBLE WITH CPAP & ORAL APPLIANCES
It has been said that with CPAP we have what's called efficacy (they work) but chase compliance (there're hard and for some impossible to wear).
TROUBLE WITH ORAL APPLIANCES
It then has to be said regarding Oral Appliances that we have compliance (they are easy to wear) yet we chase efficacy (they don't always work).
Sounds Confusing Doesn't It? Let's talk about that a moment and see if we can clear things up a bit!
- First what works for one person can but does not always work for the next.
- The most prescribed and the most efficacious therapy for treating Sleep Apnea is PAP Therapy - efficacious means successful in producing a desired result.
- The therapy that is the easiest to adhere to (wear) is the Oral Appliance but they are not as efficacious as Pap Therapy.
- But it has been argued that if CPAP is worn 1/2 the number of hours that an Oral Appliance is worn they would have equal health outcomes since to have Effectiveness both Efficacy and Compliance are required.
The graph below reflect that concept
Given The Above Is It Shocking To Think It A Challenge To Get this Right?
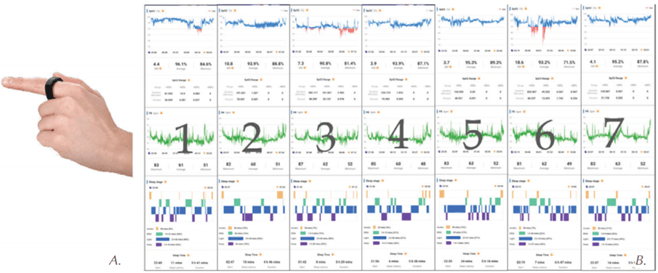
The Reality Of Technology Above
The good news is that the technological advancements we have available today and the ones we are racing towards tomorrow allow us to use simple ring type devices (upper left) and "chiclet" sized devices (upper right) that when worn allow us to monitor consecutive nights of blood oxygen (SPo2) levels and even sinc ten full nights of consecutive home Sleep Study Data (AHI & SPo2) to our cell phone for upload to a sleep physician for interpretation and treatment prescriptions.
The work above is content created by Dr. John Vivianio
Dream Station AutoPAPDream Wear Under The Nose Dream Wear Full Face Masks
If You Were To Ask Many Patients We Have Clearly Saved The Best For Last As All They Can See Is Their Attempted PAP Therapy In Their Rear View Mirror. Other Options Include:
- Oral Appliance Therapy
- Combination Therapy
- Inspire HGN Implant Stimulators
- Various Surgical Options
- Snoring